相关热词搜索: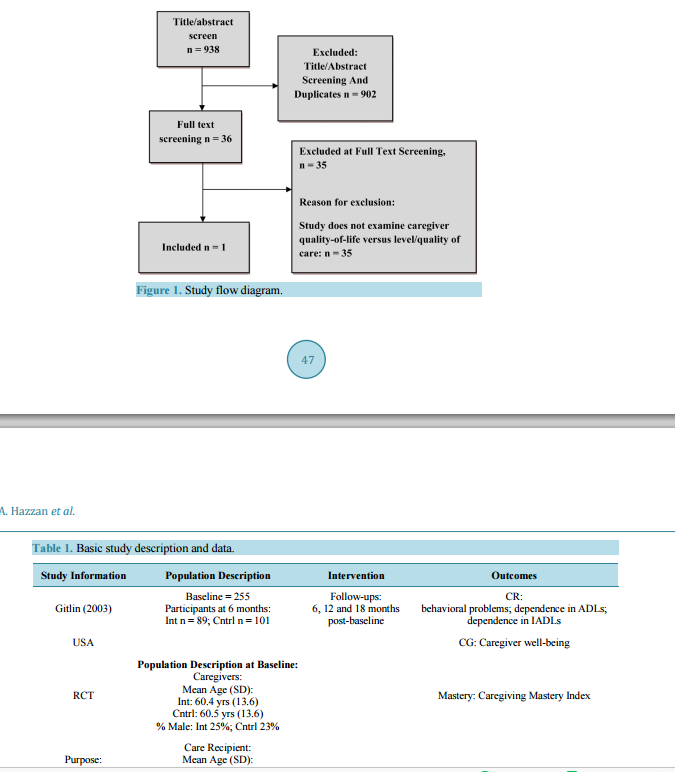 Association between Caregiver Quality of Life and the Care Provided to Persons with Alzheimer’s Disease: Systematic Review Afeez Abiola Hazzan1*, Harry Shannon1, Jenny Ploeg2, Parminder Raina1, Mark Oremus1 1 Department of Clinical Epidemiology and Biostatistics, McMaster University, Hamilton, Canada 2 School of Nursing, Faculty of Health Sciences, McMaster University, Hamilton, Canada Email: * [email protected] Received 3 February 2014; revised 1 March 2014; accepted 9 March 2014 Copyright © 2014 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract We reviewed the literature to examine whether an association exists between the quality of life (QoL) of primary informal Alzheimer"s disease (AD) caregivers and the level and quality of care that these caregivers provide to their loved ones with AD. We obtained studies focusing on the care that these caregivers provide for their family members with AD. Our outcome of interest was level or quality of care and the independent variable was caregiver QoL. We extracted data in tabular form and used a narrative synthesis approach to describe our findings. Only one relevant study was included in the review. Overall, the evidence was equivocal regarding the associations between caregiver QoL and the level/quality of care in AD. Keywords Alzheimer’s Disease Caregiver; Quality of Life; Level of Care; Quality of Care 1. Introduction Alzheimer’s disease (AD) is a type of dementia characterized by progressive declines in cognitive and functional abilities [1]. Its symptoms often begin with memory loss and progress to an inability to perform basic activities of daily living (e.g., dressing, feeding); persons with AD eventually become completely reliant on thirdparty care [2]. * Corresponding author. A. A. Hazzan et al. 45 The impact of AD is global. An estimated 5.4 million people in the United States had AD in 2012, including 5.2 million people aged 65 and older [3]. In Canada, projections show the number of cases of AD could increase to 509,000 in 2031 from the current figure of 300,000 [4] [5]. Also, the proportion of people living with dementia in North America will increase to 63% over the next twenty years [6]. About 36 million people world-wide were living with AD in 2010 and this figure is set to top 115 million people by 2050 [4]. Further estimates suggest that AD will affect nearly 1 in every 85 people around the world over the next 40 years [6]. Caregivers provide critically needed care for persons with AD because cognitive decline ultimately prevents people diagnosed with AD from functioning independently. Primary informal caregivers (e.g., spouses, children) are generally not paid for the care they provide. These caregivers perform comprehensive duties such as shopping for groceries, helping with medications, managing finances and legal affairs, guarding against wandering and other unsafe practices, bathing, dressing, and making arrangements for medical care [7]. Even when persons with AD move to assisted living facilities, most primary caregivers continue to provide help with grooming [8] [9]. Due to the many tasks required of AD caregivers, the emotional and physical demands of caregiving are high. Consequently, unpaid family caregivers in AD usually have lower QoL than caregivers for persons who have not been diagnosed with AD [10]. Since lower QoL has been shown to increase work absenteeism and reduce productivity in workplace settings [11], it is possible that the demands of caregiving might also lead to declining “caregiver productivity” in care provision. We hypothesized that caregiver QoL might affect caregivers’ ability to provide care. Indeed, the strain of performing caregiver tasks has been cited as one of the leading reasons why caregivers institutionalize their loved ones [12] [13]. The current review investigated the association between the QoL of primary informal AD caregivers and the level and quality of care that these caregivers provide to their loved ones with AD. We addressed the following research questions: What is the relationship between caregiver QoL and level of care? What is the relationship between caregiver QoL and quality of care? 2. Methods 2.1. Data Sources and Selection A protocol detailing the methods for this systematic review has been previously published (PROSPERO registration number: CRD42013003613) [14]. Briefly, we searched CINAHL, Cochrane Central-OVID, EmbaseOVID, Medline-OVID, PsycINFO-OVID and Business Source Complete from database inception through December 2012. The search strategy was adjusted for the specific nuances of each database. Internet searches were also performed in order to identify grey literature. An experienced medical librarian conducted the literature search (databases and internet) and uploaded the results to DistillerSR. DistillerSR is an online application specifically designed for conducting the screening and data extraction phases of systematic reviews. Standardized screening forms were developed for this study and uploaded onto Distiller. All screening and data extraction were done on DistillerSR. Titles and abstracts of studies identified in the literature search were independently screened by two reviewers. Studies meeting the eligibility criteria, or studies whose titles and abstracts did not provide sufficient information to assess eligibility, advanced to full-text screening. During full-text screening, two reviewers independently read each entire paper and assessed eligibility. Conflicts were resolved through reviewer consensus or by the involvement of a third reviewer. 2.2. Criteria for Considering Studies for This Review We included studies dealing with primary informal caregivers of community-dwelling persons with AD. We included studies with QoL as the independent variable and outcomes pertaining to level or quality of care. Quality-of-Life (QoL) The concept of QoL may be defined in several ways. The World Health Organization defines QoL to refer to a person’s state of complete physical, mental, and social well-being [15]. Though complex to describe, QoL has often been defined as “the degree to which a person enjoys the important possibilities of his or her life” [16]. QoL may be measured using scales, several of which have been developed for healthcare research [17]. Other A. A. Hazzan et al. 46 generic, health-related QoL scales include the Short Form 36 (SF-36) [18], Euro QoL Group’s EQ-5D [19], and the World Health Organization Quality of Life-BREF [20]. We included any study measuring caregiver QoL, regardless of how the construct was defined or measured. In addition to QoL, studies examining the impact of constructs that are closely related to QoL (e.g., well-being, social support, caregiver burden, depression) were treated as if they measured QoL. 2.3. Definition of Concepts Related to QoL 2.3.1. Caregiver Well-Being The concept of well-being is closely related to QoL. In the context of care giving, it is concerned with caregivers" basic human needs and their satisfaction with activities of daily living. Caregiver well-being has several components including social, physical, emotional, and spiritual [15]. In health research, well-being is generally measured by asking respondents to evaluate their state over a given period of time. 2.3.2. Social Support Social support is a multidimensional construct of the extent to which inpiduals receive emotional support, assistance, information, guidance and feedback, personal support, and companionship from family members, friends, co-workers, other persons (for example, acquaintances, religious leaders, therapists), or organizations (for example, caregiver support groups) [21]. 2.3.3. Caregiver Burden Caregiver burden is an important component of QoL. It is operationalized by any construct representing the physical, emotional, and financial strain of providing care for a loved one with AD. The Zarit Burden Interview (ZBI) is a widely used instrument for measuring caregiver burden [10] [22]. 2.3.4. Caregiver Depression Although depression is a key element of QoL, it is also an important construct on its own. Indeed, depression is one of the common side effects of long-term care giving [23]. Depression can be measured by several instruments, including the Center for Epidemiologic Studies-Depression (CES-D) scale [24] [25]. 2.3.5. Caregiver Sleep There is a strong association between sleep disturbances and depression which impacts quality of life [26]. Caregivers of persons with AD generally report high level of sleep problems, and the Caregiver Sleep Questionnaire is a common way to measure the quality, quantity, and the frequency of seven sleep problems during the past month [27]. 2.4. Definition of Level/Quality of Care 2.4.1. Level of Care Level of care outcomes were measured as total hours per day that caregivers were doing things for care recipients (CR) and total hours per day that caregivers were helping CR with Instrumental Activities of Daily Living (IADLs) (“About how many hours a day do you estimate that you are actually doing things for care recipient?”). 2.4.2. Quality of Care Quality of care outcomes were measured as caregiver proficiency in care giving. Proficiency included caregiver mastery (“How often do you feel you should be doing more for care recipient?”) and skill enhancement as measured by the Task Management Strategy Index or TMSI (“To what extent were positive care giving strategies used to manage activities of daily living [ADL], dependence and problem behaviors?”). 2.5. Assessment of Risk of Bias and Grade Each included study was assessed for risk of bias by two raters using the Cochrane Risk of Bias Tool v5.1 [28]-[30]. We rated risk of bias on the three domains identified in the tool, namely blinding of outcome assessment, incomplete outcome data, and selective reporting. The overall risk of bias was judged by using the ratings on the A. A. Hazzan et al. 47 inpidual domains and any instructions for overall assessment that the tool might contain. The overall risk of bias was classified as “low”, “high”, or “unclear”. In addition to assessing the risk of bias, we also used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) to rate the level of evidence and to make judgements regarding whether the evidence is convincing enough already, such that future evidence is unlikely to change our conclusions. Studies were rated on the type of evidence (for example, RCT or observational), consistency, directness, precision and quality. The overall GRADE score, which reflects the average of the ratings on each of the dimensions above, was categorized as “high”, “moderate”, “low”, and “very low” [31]. 2.6. Data Extraction A data extraction form was developed to collect the following information from included articles: study characteristics, participant characteristics (e.g., type and number of caregivers and care recipients, caregiver relationship to care recipient, living situation, age, AD diagnostic criteria), and results (e.g., quality of life, quality of care, level of care). The data extraction form was piloted by two reviewers and further refined as necessary. Two reviewers independently extracted all data and met to resolve discrepancies by consensus. Whenever consensus could not be reached, a third reviewer was asked to adjudicate. In cases where studies reported outcome results over different time periods, we extracted data from each time period to examine the impact of the intervention over time. We followed the PRISMA guidelines in completing this systematic review [32]. 3. Results Figure 1 shows the flow of studies through the screening process. Nine hundred thirty-eight articles were captured during the initial literature search, of which 902 (96%) were excluded at the title and abstract screening stage. Full text screening was performed on 36 articles, of which only one was found to meet all the inclusion criteria. The reason for exclusion at the full-text screening stage was non-relevance of the article to our research objective (e.g., the outcomes of interest were not measured). Table 1 shows detailed study information for the only included study [33]. 3.1. Methodological Quality Assessment The included study, by Gitlin et al. [33], is an RCT in which outcome data were completely presented and no issues were evident with respect to selective reporting or any other type of bias. Overall, the study was rated as having a “low risk” of bias. Figure 1. Study flow diagram. A. A. Hazzan et al. 48 Table 1. Basic study description and data. Study Information Population Description Intervention Outcomes Gitlin (2003) Baseline = 255 Participants at 6 months: Int n = 89; Cntrl n = 101 Follow-ups: 6, 12 and 18 months post-baseline CR: behavioral problems; dependence in ADLs; dependence in IADLs USA CG: Caregiver well-being RCT Population Description at Baseline: Caregivers: Mean Age (SD): Int: 60.4 yrs (13.6) Cntrl: 60.5 yrs (13.6) % Male: Int 25%; Cntrl 23% Mastery: Caregiving Mastery Index Purpose: ESP–2 phases–active (first 6 months); maintenance (next 6 months) Care Recipient: Mean Age (SD): Int: 80.2 yrs (8.0) Cntrl: 81.5 yrs (8.0) % Male: Int 28%; Cntrl 37% Mean MMSE (SD): Int 11.6 (7.3); Cntrl 12.5 (7.1) Skill enhancement: Task Management Strategy Index CG = caregiver; CR = care recipient; ESP = environmental skill-building program; NH = nursing home; Int = intervention; Cntrl = control; MMSE = mini-mental state examination; ADL = Activities of daily living; IADL; Instrumental activities of daily living. 3.2. Summary of Extracted Study Although the included study was not specifically designed to answer our research questions, the data contained in the study did indirectly address whether caregiver QoL impacts the level or quality of care that caregivers provide to loved ones with AD. The Gitlin et al paper was primarily designed to examine the effect of an intervention (skills building program versus usual care) on caregiver well-being and care recipient functioning but contains sufficient information to examine the relationship between QoL and level/quality of care within groups of caregivers randomized into intervention and usual care control groups. Table 1 presents demographic information from the Gitlin et al. [33] paper that is relevant to the research questions in the current study. The population examined by Gitlin et al. consisted of 255 primary informal AD caregivers who were providing care for at least four hours per day for 6 months or more. The authors evaluated the impact of a Home Environmental Skill-Building Program (ESP) compared to a usual care control group. The ESP was designed to provide caregivers with education, problem-solving skills, and adaptive equipment to manage daily care challenges effectively and to reduce burdensome environmental stressors (e.g., CR behaviors) [33]. One hundred ninety caregivers completed six months of follow-up. As part of the study, the authors collected information about caregiver overall well-being, an important component of QoL [15] [33]. Caregiver overall well-being was measured with a 13-item scale (the Perceived Change Index [PCI]). On the PCI, caregivers used a 5-point scale to rate whether their situation (e.g., ability to manage difficult behaviors) ranged from “becoming worse” to “improving a lot” over the past month. The relevant level of care measure in the Gitlin et al. paper was caregiver time (the amount of time devoted to providing care and total hours of IADL help). The quality of care measures included caregiver mastery and skill enhancement. Caregiver mastery was measured with the Caregiving Mastery Index (CMI) [33]. The CMI is a six-item scale evaluating the caregiver’s appraisal of his or her ability to provide care to the CR (e.g., “How often do you feel you should be doing more for care recipient?). The scale uses a 5-point Likert format ranging from 1 (never) to 5 (always). A higher score means greater mastery of the care giving role. Skill enhancement was measured with the Task Management Strategy Index (TMSI), which is a 19-item scale that measures the extent to which positive care giving strategies were used to manage ADL dependence and problem behaviors in care recipients. The scale uses a 5-point Likert format from 1 (never) to 5 (always) [33]. 3.2.1. What Is the Relationship between Caregiver QoL and Level or Quality of Care Provided to Persons with AD? Table 2 shows the summary of data extracted from the included study. Overall, results from this study are A. A. Hazzan et al. 49 Table 2. Association between QoL and level/quality of care. Type of variable Measure Experimental Control BE 6ME Diff E BC 6MC Diff C QoL (Overall well-being) PCI 2.84 3.00 0.16 2.94 2.89 −0.05 Level of care Hours doing things for CR 12.23 11.51 −0.79 12.13 11.66 −0.47 Level of care Hours helping with IADLs 5.25 5.50 0.25 6.03 5.62 −0.41 Quality of care TMSI 2.91 3.05 0.14 2.92 2.93 0.01 Quality of care CMI 3.74 3.88 0.14 3.87 3.84 −0.03 E = Experimental; C = Control; CR = Care Recipient; QoL = Quality of Life; IADL = Instrumental Activities of Daily Living; PCI = Perceived Change Index; TMSI = Task Management Strategy Index; CMI = Care giving Mastery Index; B = Baseline; 6M = 6 month follow-up; Diff = Difference. mixed. We are primarily interested in whether changes in QoL are associated with changes in level or quality of care, within the experimental and the control group. Comparisons are described below: 3.2.2. Experimental vs Control Group: Baseline and 6-Month Follow-up Comparing the experimental group to the control group on outcomes related to level of care at baseline, results related to hours doing things for the CR are consistent with the hypothesis since lower QoL at baseline (before any intervention is given) is associated with higher number of hours spent caring for the CR (someone spending a lot of time providing care will have lower QoL). However, results for hours helping with IADLs do not support the hypothesis. Results for the quality of care variables (TMSI and CMI) are also consistent with the hypothesis. Compared to caregivers in the control group, lower QoL among caregivers in the intervention group is consistent with the lower quality of care that these caregivers provide at baseline. After 6 months of follow-up, there was an increase in the mean QoL among caregivers in the experimental group. On the other hand, there was a decrease in the mean QoL of caregivers in the control group over this period of time. Consistent with the hypothesis, there was an increase in the level (Hours helping with IADLs) and quality of care (TMSI and CMI) provided by caregivers in the intervention group compared to caregivers in the control group. The only exception to this trend is “hours doing things for CR”, which decreased among intervention group caregivers. 3.2.3. Experimental Group: Baseline to 6-Month Follow up Among caregivers in the experimental group, the QoL (PCI) variable increased over time. The overall results for this group from baseline to 6-months show that the experimental group QoL and quality of care measures increased over the follow-up period. On the other hand, results for the level of care variables are mixed, with hours doing things for CR showing a reduction over time, and hours helping with IADLs showing an increase over the same time period. The overall trend is consistent with the hypothesis since higher QoL at 6-month follow-up is related to higher level of care and quality of care. This means that caregivers with higher QoL are more likely to provide higher level of care and better quality of care. 3.2.4. Control: Baseline to 6-Month Follow up For caregivers in the control group, the QoL decreased over time from baseline to follow-up. The level of care and quality of care variables also decreased over time, with the only exception being TMSI which remains fairly constant over time. The observed trend is also consistent with the hypothesis since caregivers with lower QoL are likely to provide lower level and quality of care. Compared to caregivers in the control group, caregivers in the experimental group provided better care overall after 6-months follow-up. A. A. Hazzan et al. 50 3.3. Grade Results from the GRADE assessment are presented in Table 3. For both the level and quality of care outcomes, the type of evidence presented received the highest rating because the included study (Gitlin et al.) is an RCT and there were no serious issues with the quality of the study. However, the consistency, directness, and precision scores for both outcomes are affected by different factors, resulting in reduced scores on some of these domains. Consistency and directness points were deducted from both outcomes because the study was not designed to answer our research questions and results only indirectly addressed the questions. Finally, the precision scores were unchanged because the measures of effect were not statistically significant as reported in the included study [34]. 4. Discussion We were interested in evaluating how caregiver QoL impacts the level or quality of care that primary informal caregivers provide to their loved ones with AD. The included paper looks at level of care outcomes such as hours doing things for the CR and hours helping with IADLs. The paper also examine quality of care outcomes such as skill enhancement and caregiver mastery. Overall, the evidence was equivocal regarding the relationship between caregiver QoL and the level/quality of care provided to persons with AD. This is also the reason why the overall GRADE ratings for the outcomes from these studies are “moderate” This means that further research is likely to have an important impact on our confidence in this result [34]. Although the overall results were mixed, this study shows that higher caregiver QoL is related to higher level and quality of care provided to persons with AD. Among a group of 255 primary informal AD caregivers who were providing care for at least four hours per day for 6 months or more, findings at baseline show that caregivers spending a lot of time providing care were more likely to have lower QoL. This supports previous studies that have shown that caregiving in AD is stressful and has serious implications for the well-being of unpaid family caregivers [7]-[10]. In order to shed light on the relationship between QoL and level/quality of care provided to persons with AD, results for intervention and control group caregivers were analyzed after 6-months of follow-up. While there was an increase in the mean QoL among caregivers in the intervention group over the 6-month follow-up period, there was a decrease in the mean QoL of caregivers in the control group. As the QoL of intervention group caregivers increases over time, there was an increase in the level of care (Hours helping with IADLs) among these caregivers relative to caregivers in the control group. However, there was a decrease in the other level of care (Hours doing things for the CR) variable after 6-month of follow-up. It should be noted that “hours helping with IADLs” is a component of “total hours doing things for the CR” [33]. It is possible that “hours helping with IADLs” captures the important duties that AD caregivers perform for their loved ones better than “hours doing things for the CR”. At the same time, there was an increase in the quality of care (TMSI and CMI) provided by caregivers in the intervention group compared to those in the control group after 6-month follow-up. Although some specific results were mixed, the overall results supports the hypothesis that better caregiver QoL may lead to better level/quality of care for the CR. The mixed evidence from this systematic review suggests that research is needed to examine the relationship between caregiver QoL and the care provided to persons with AD. It is important to understand this relationship because our healthcare system places great responsibility on AD caregivers and we already know that AD caregivers’ QoL is lower than other caregivers’ QoL. Considering the critical duties that caregivers of persons with Table 3. Grade results. Outcome Type of evidence Quality Consistency Directness Precision GRADE Notes Level of care (hours helping care recipient, hours helping with IADLs) 4 0 −1 −1 0 Moderate Directness point deducted because results indirectly address review questions Quality of care (TMSI, CMI) 4 0 −1 −1 0 Moderate Consistency point deducted because only one trial examined the intervention IADL = Instrumental Activities of Daily Living; TMSI = Task Management Strategy Index; CMI = Care giving Mastery Index. A. A. Hazzan et al. 51 AD perform, the current systematic review shows an urgent need for studies examining the relationships between caregiver QoL and the level/quality of care. The ideal type of primary study to address our research questions is a longitudinal cohort study measuring QoL, level of care, and quality of care in AD caregivers. If such a study were to be conducted, the longitudinal component will show how the relationship between variables changes as caregiver QoL deteriorates over time. The Canadian Longitudinal Study on Aging (CLSA) is a model for the types of studies that could be used to collect the data needed to answer our research questions [35] [36]. If the results from a longitudinal study show that caregivers’ QoL does indeed affect their ability to provide care for their loved ones with AD, then this issue needs to be addressed through additional support programs that improve caregiver QoL. For example, respite care and similar alternative care options could be made more available to relieve caregivers of persons with AD from their care giving duties. Further, programs could be designed to help caregivers address day-to-day challenges such as financial and legal planning, stress management, and behavioural interventions. Access to educational interventions that help caregivers acquire valuable skills would also improve the care giving experience. 5. Limitations One limitation of this systematic review is that the only study that met the inclusion criteria provided indirect evidence to answer the research questions. Also, because primary data were not available, it was not possible to determine if the observed relationships between caregiver QoL and level/quality of care are statistically significant or not. However, this systematic review makes an important contribution to the literature because it shows that very little research has been conducted into the relation between QoL and level/quality of care. The review highlights the need for additional research in this area. 6. Conclusion As population aging continues to occupy a more prominent role in research and policy discussions, more attention needs to be given to the situation of unpaid family caregivers of persons with AD. Family caregivers play an important role in the management of AD and several studies have shown that these caregivers experience lower QoL compared to the QoL experienced by caregivers of persons who do not have AD. This systematic review shows that there is insufficient evidence regarding the nature of the relationship between unpaid family caregiver QoL and level/quality of care provided to persons with AD. Considering the important duties that caregivers of persons with AD perform, additional research should be conducted to examine this relationship. Acknowledgements The authors would like to thank Mary Gauld for helping with Distiller and article screening. We thank Maureen Rice for helping with developing the literature search strategies and conducting the literature search. We also thank Vincent Wu and Arnav Agarwal for helping with article screening. References [1] Alzheimer’s Disease International (2011) World Alzheimer Report 2011. The Benefits of Early Diagnosis and Intervention. Alzheimer’s Disease International, London. http://www.alz.co.uk/research/world-report-2011/ [2] Burns, A. and Iliffe, S. (2009) Alzheimer’s Disease. British Medical Journal, 338, 46-471. http://dx.doi.org/10.1136/bmj.b46 [3] Hebert, L.E., Scherr, P.A., Bienias, J.L., Bennett, D.A. and Evans, D.A. (2003) Alzheimer disease in the US Population: Prevalence estimates Using the 2000 Census. Archives of Neurology, 60, 1119-1122. http://dx.doi.org/10.1001/archneur.60.8.1119 [4] Alzheimer Society of Canada (2012) Key Facts about Alzheimer’s Disease and Related Dementia-Prevalence Figures. Alzheimer Society of Canada, Toronto. http://www.alzheimer.ca/english/disease/stats-intro.htm [5] Canadian Study of Health and Aging (1994) Canadian Study of Health and Aging: Study Methods and Prevalence of Dementia. Canadian Medical Association Journal, 150, 899-913. [6] Prince, M. and Jackson, J. (2009) Alzheimer’s Disease International: World Alzheimer Report. A. A. Hazzan et al. 52 http://www.alz.co.uk/research/world-report [7] deMoraes, S.R. and da Silva., L.S. (2009) An Evaluation of the Burden of Alzheimer Patients on Family Caregivers. Cadernos de Saúde Pública, 25, 1807-1815. [8] Schulz, R., Belle, S.H., Czaja S.J, McGinnis, K.A., Stevens, A. and Zhang, S. (2004) Long-Term Care Placement of Dementia Patients and Caregiver Health and Well-Being. The Journal of the American Medical Association, 292, 961-967. http://dx.doi.org/10.1001/jama.292.8.961 [9] Port, C.L., Zimmerman, S., Williams, C.S., Dobbs, D., Preisser, J.S. and Williams, S.W. (2005) Families Filling The Gap: Comparing Family Involvement for Assisted Living and Nursing Home Residents with Dementia. Gerontologist, 1, 87-95. [10] Zarit, S.H., Orr, N.K. and Zarit, J.M. (1985) The Hidden Victims of Alzheimer’s Disease: Families under Stress. New York University Press, New York. [11] Bolge, S.C., Doan, J.F., Kannan, H. and Baran, R.W. (2009) Association of Insomnia with Quality of Life, Work Productivity, and Activity Impairment. Quality of Life Research, 18, 415-422. http://dx.doi.org/10.1007/s11136-009-9462-6 [12] Gaugler, J.E., Yu, F., Krichbaum, K. and Wyman, J.F. (2009) Predictors of Nursing Home Admission for Persons with Dementia. Medical Care, 47, 191-198. http://dx.doi.org/10.1097/MLR.0b013e31818457ce [13] Alzheimer’s Association and National Alliance for Care Giving (2004) Families Care: Alzheimer’s Disease Care Giving in the United States. www.alz.org [14] Hazzan, A.A., Ploeg, J., Shannon, H., Raina, P., Oremus, M. (2013) Association between Caregiver Quality of Life and the Care Provided to Persons with Alzheimer’s Disease: Protocol for a Systematic. Systematic Review, 13, 17. [15] World Health Organization (WHO) (1997) Measuring Quality of Life. WHOQOL. World Health Organization, Geneva. [16] Susniene, D. and Jurkauksa, A. (2009) The Concepts of Quality of Life and Happiness—Correlation and Differences. Engineering Economics. [17] McSweeny, A.J. and Creer, T.L. (1995) Health-Related Quality-Of-Life Assessment in Medical Care. Diseasea-Month, 41, 1-71. [18] Ware, J.E. and Sherbourne, C.D. (1992) The MOS 36-Item Short-Form Health Survey (SF-36) Conceptual Framework and Item Selection. Medical Care, 30, 473-483. http://dx.doi.org/10.1097/00005650-199206000-00002 [19] EuroQol Group (1990) EuroQol—A New Facility for the Measurement of Health-Related Quality Of Life. The Euro Qol Group. Health Policy, 16, 199-208. http://dx.doi.org/10.1016/0168-8510(90)90421-9 [20] Saxena, S. and Orley, J. (1997) Quality of Life Assessment: The World Health Organization Perspective. European Psychiatry, 12, 263s-266s. http://dx.doi.org/10.1016/S0924-9338(97)89095-5 [21] Markowitz, J.S., Gutterman, E.M., Sadik, K. and Papadopoulos, G. (2003) Health-Related Quality of Life for Caregivers of Patients with Alzheimer Disease. Alzheimer Disease and Associated Disorders, 17, 209-214. http://dx.doi.org/10.1097/00002093-200310000-00003 [22] Bédard, M., Molloy, D.W., Squire, L., Dubois, S., Lever, J.A. and O’Donnell, M. (2001) The Zarit Burden Interview: A New Short Version and Screening Version. Gerontologist, 41, 652-657. http://dx.doi.org/10.1093/geront/41.5.652 [23] Ferro, M.A. and Speechley, K.N. (2009) Depressive Symptoms among Mothers of Children with Epilepsy: A Review of Prevalence, Associated Factors, and Impact on Children. Epilepsia, 50, 2344-2354. http://dx.doi.org/10.1111/j.1528-1167.2009.02276.x [24] Radloff, L.S. (1977) The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement, 1, 385-401. http://dx.doi.org/10.1177/014662167700100306 [25] Niedhammer, I., David, S. and Degioanni, S. (2006) Association between Workplace Bullying and Depressive Symptoms in the French Working Population. Journal of Psychosomatic Research, 61, 251-259. http://dx.doi.org/10.1016/j.jpsychores.2006.03.051 [26] Teri, L., McCurry, S.M., Logsdon, R. and Gibbons, L.E. (2005) Training Community Consultants to Help Family Members Improve Dementia Care: A Randomized Controlled Trial. Gerontologist, 45, 802-811. http://dx.doi.org/10.1093/geront/45.6.802 [27] McCurry, S.M. and Teri, L. (1995) Sleep Disturbance in Elderly Caregivers of Dementia Patients. Clinical Gerontologist, 16, 51-66. http://dx.doi.org/10.1300/J018v16n02_05 [28] Higgins, J.P., Altman, D.G., Gøtzsche, P.C., Jüni, P., Moher, D., Oxman, A.D., Savovic, J., Schulz, K.F., Weeks, L., Sterne, J.A., Cochrane Bias Methods Group and Cochrane Statistical Methods Group. (2011) The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. British Medical Journal, 343, d5928. http://dx.doi.org/10.1136/bmj.d5928 A. A. Hazzan et al. 53 [29] Cochrane Effective Practice and Organisation of Care Group Draft Risk of Bias Tool (2011) Wiley, Oxford. http://epoccochrane.org/epocresources-review-authors [30] Hartling, L., Bond, K., Harvey, K., Santaguida, P.L., Viswanathan, M. and Dryden, D.M. (2010) Developing and Testing a Tool for the Classification of Study Designs in Systematic Reviews of Interventions and Exposures. http://www.ncbi.nlm.nih.gov/books/NBK52670/pdf/TOC.pdf [31] The Cochrane Handbook for Systematic Reviews of Intervention. (2011) The GRADE Approach. Chapter 12.2.1. http://handbook.cochrane.org/chapter_12/12_2_1_the_grade_approach.htm [32] Moher, D., Liberati, A., Tetzlaff, J. and Altman, D.G. (2010) PRISMA Group: Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. International Journal of Surgery, 8, 336-341. http://dx.doi.org/10.1016/j.ijsu.2010.02.007 [33] Gitlin, L.N., Winter, L., Corcoran, M., Dennis, M.P., Schinfeld, S. and Hauck, W.W. (2003) Effects of the Home Environmental Skill-Building Program on the Caregiver-Care Recipient Dyad: 6-Month Outcomes from the Philadelphia REACH Initiative. Gerontologist, 43, 532-546. http://dx.doi.org/10.1093/geront/43.4.532 [34] Guyatt, G.H., Oxman, A.D., Vist, G.E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., Schünemann, H.J. and GRADE Working Group. (2008) GRADE: An Emerging Consensus on Rating Quality of Evidence and Strength of Recommendations. British Medical Journal, 336, 924-926. http://dx.doi.org/10.1136/bmj.39489.470347.AD [35] Canadian Study of Health and Aging Working Group. (2000) The Incidence of Dementia in Canada. Neurology, 55, 66-73. http://dx.doi.org/10.1212/WNL.55.1.66 [36] Raina, P.S., Wolfson, C., Kirkland, S.A., Griffith, L.E., Oremus, M., Patterson, C., Tuokko, H., Penning, M., Balion, C.M., Hogan, D., Wister, A., Payette, H., Shannon, H. and Brazil, K. (2009) The Canadian Longitudinal Study on Aging (CLSA). Canadian Journal on Aging, 28, 221-229. http://dx.doi.org/10.1017/S0714980809990055
Association between Caregiver Quality of Life and the Care Provided to Persons with Alzheimer’s Disease: Systematic Review Afeez Abiola Hazzan1*, Harry Shannon1, Jenny Ploeg2, Parminder Raina1, Mark Oremus1 1 Department of Clinical Epidemiology and Biostatistics, McMaster University, Hamilton, Canada 2 School of Nursing, Faculty of Health Sciences, McMaster University, Hamilton, Canada Email: * [email protected] Received 3 February 2014; revised 1 March 2014; accepted 9 March 2014 Copyright © 2014 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract We reviewed the literature to examine whether an association exists between the quality of life (QoL) of primary informal Alzheimer"s disease (AD) caregivers and the level and quality of care that these caregivers provide to their loved ones with AD. We obtained studies focusing on the care that these caregivers provide for their family members with AD. Our outcome of interest was level or quality of care and the independent variable was caregiver QoL. We extracted data in tabular form and used a narrative synthesis approach to describe our findings. Only one relevant study was included in the review. Overall, the evidence was equivocal regarding the associations between caregiver QoL and the level/quality of care in AD. Keywords Alzheimer’s Disease Caregiver; Quality of Life; Level of Care; Quality of Care 1. Introduction Alzheimer’s disease (AD) is a type of dementia characterized by progressive declines in cognitive and functional abilities [1]. Its symptoms often begin with memory loss and progress to an inability to perform basic activities of daily living (e.g., dressing, feeding); persons with AD eventually become completely reliant on thirdparty care [2]. * Corresponding author. A. A. Hazzan et al. 45 The impact of AD is global. An estimated 5.4 million people in the United States had AD in 2012, including 5.2 million people aged 65 and older [3]. In Canada, projections show the number of cases of AD could increase to 509,000 in 2031 from the current figure of 300,000 [4] [5]. Also, the proportion of people living with dementia in North America will increase to 63% over the next twenty years [6]. About 36 million people world-wide were living with AD in 2010 and this figure is set to top 115 million people by 2050 [4]. Further estimates suggest that AD will affect nearly 1 in every 85 people around the world over the next 40 years [6]. Caregivers provide critically needed care for persons with AD because cognitive decline ultimately prevents people diagnosed with AD from functioning independently. Primary informal caregivers (e.g., spouses, children) are generally not paid for the care they provide. These caregivers perform comprehensive duties such as shopping for groceries, helping with medications, managing finances and legal affairs, guarding against wandering and other unsafe practices, bathing, dressing, and making arrangements for medical care [7]. Even when persons with AD move to assisted living facilities, most primary caregivers continue to provide help with grooming [8] [9]. Due to the many tasks required of AD caregivers, the emotional and physical demands of caregiving are high. Consequently, unpaid family caregivers in AD usually have lower QoL than caregivers for persons who have not been diagnosed with AD [10]. Since lower QoL has been shown to increase work absenteeism and reduce productivity in workplace settings [11], it is possible that the demands of caregiving might also lead to declining “caregiver productivity” in care provision. We hypothesized that caregiver QoL might affect caregivers’ ability to provide care. Indeed, the strain of performing caregiver tasks has been cited as one of the leading reasons why caregivers institutionalize their loved ones [12] [13]. The current review investigated the association between the QoL of primary informal AD caregivers and the level and quality of care that these caregivers provide to their loved ones with AD. We addressed the following research questions: What is the relationship between caregiver QoL and level of care? What is the relationship between caregiver QoL and quality of care? 2. Methods 2.1. Data Sources and Selection A protocol detailing the methods for this systematic review has been previously published (PROSPERO registration number: CRD42013003613) [14]. Briefly, we searched CINAHL, Cochrane Central-OVID, EmbaseOVID, Medline-OVID, PsycINFO-OVID and Business Source Complete from database inception through December 2012. The search strategy was adjusted for the specific nuances of each database. Internet searches were also performed in order to identify grey literature. An experienced medical librarian conducted the literature search (databases and internet) and uploaded the results to DistillerSR. DistillerSR is an online application specifically designed for conducting the screening and data extraction phases of systematic reviews. Standardized screening forms were developed for this study and uploaded onto Distiller. All screening and data extraction were done on DistillerSR. Titles and abstracts of studies identified in the literature search were independently screened by two reviewers. Studies meeting the eligibility criteria, or studies whose titles and abstracts did not provide sufficient information to assess eligibility, advanced to full-text screening. During full-text screening, two reviewers independently read each entire paper and assessed eligibility. Conflicts were resolved through reviewer consensus or by the involvement of a third reviewer. 2.2. Criteria for Considering Studies for This Review We included studies dealing with primary informal caregivers of community-dwelling persons with AD. We included studies with QoL as the independent variable and outcomes pertaining to level or quality of care. Quality-of-Life (QoL) The concept of QoL may be defined in several ways. The World Health Organization defines QoL to refer to a person’s state of complete physical, mental, and social well-being [15]. Though complex to describe, QoL has often been defined as “the degree to which a person enjoys the important possibilities of his or her life” [16]. QoL may be measured using scales, several of which have been developed for healthcare research [17]. Other A. A. Hazzan et al. 46 generic, health-related QoL scales include the Short Form 36 (SF-36) [18], Euro QoL Group’s EQ-5D [19], and the World Health Organization Quality of Life-BREF [20]. We included any study measuring caregiver QoL, regardless of how the construct was defined or measured. In addition to QoL, studies examining the impact of constructs that are closely related to QoL (e.g., well-being, social support, caregiver burden, depression) were treated as if they measured QoL. 2.3. Definition of Concepts Related to QoL 2.3.1. Caregiver Well-Being The concept of well-being is closely related to QoL. In the context of care giving, it is concerned with caregivers" basic human needs and their satisfaction with activities of daily living. Caregiver well-being has several components including social, physical, emotional, and spiritual [15]. In health research, well-being is generally measured by asking respondents to evaluate their state over a given period of time. 2.3.2. Social Support Social support is a multidimensional construct of the extent to which inpiduals receive emotional support, assistance, information, guidance and feedback, personal support, and companionship from family members, friends, co-workers, other persons (for example, acquaintances, religious leaders, therapists), or organizations (for example, caregiver support groups) [21]. 2.3.3. Caregiver Burden Caregiver burden is an important component of QoL. It is operationalized by any construct representing the physical, emotional, and financial strain of providing care for a loved one with AD. The Zarit Burden Interview (ZBI) is a widely used instrument for measuring caregiver burden [10] [22]. 2.3.4. Caregiver Depression Although depression is a key element of QoL, it is also an important construct on its own. Indeed, depression is one of the common side effects of long-term care giving [23]. Depression can be measured by several instruments, including the Center for Epidemiologic Studies-Depression (CES-D) scale [24] [25]. 2.3.5. Caregiver Sleep There is a strong association between sleep disturbances and depression which impacts quality of life [26]. Caregivers of persons with AD generally report high level of sleep problems, and the Caregiver Sleep Questionnaire is a common way to measure the quality, quantity, and the frequency of seven sleep problems during the past month [27]. 2.4. Definition of Level/Quality of Care 2.4.1. Level of Care Level of care outcomes were measured as total hours per day that caregivers were doing things for care recipients (CR) and total hours per day that caregivers were helping CR with Instrumental Activities of Daily Living (IADLs) (“About how many hours a day do you estimate that you are actually doing things for care recipient?”). 2.4.2. Quality of Care Quality of care outcomes were measured as caregiver proficiency in care giving. Proficiency included caregiver mastery (“How often do you feel you should be doing more for care recipient?”) and skill enhancement as measured by the Task Management Strategy Index or TMSI (“To what extent were positive care giving strategies used to manage activities of daily living [ADL], dependence and problem behaviors?”). 2.5. Assessment of Risk of Bias and Grade Each included study was assessed for risk of bias by two raters using the Cochrane Risk of Bias Tool v5.1 [28]-[30]. We rated risk of bias on the three domains identified in the tool, namely blinding of outcome assessment, incomplete outcome data, and selective reporting. The overall risk of bias was judged by using the ratings on the A. A. Hazzan et al. 47 inpidual domains and any instructions for overall assessment that the tool might contain. The overall risk of bias was classified as “low”, “high”, or “unclear”. In addition to assessing the risk of bias, we also used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) to rate the level of evidence and to make judgements regarding whether the evidence is convincing enough already, such that future evidence is unlikely to change our conclusions. Studies were rated on the type of evidence (for example, RCT or observational), consistency, directness, precision and quality. The overall GRADE score, which reflects the average of the ratings on each of the dimensions above, was categorized as “high”, “moderate”, “low”, and “very low” [31]. 2.6. Data Extraction A data extraction form was developed to collect the following information from included articles: study characteristics, participant characteristics (e.g., type and number of caregivers and care recipients, caregiver relationship to care recipient, living situation, age, AD diagnostic criteria), and results (e.g., quality of life, quality of care, level of care). The data extraction form was piloted by two reviewers and further refined as necessary. Two reviewers independently extracted all data and met to resolve discrepancies by consensus. Whenever consensus could not be reached, a third reviewer was asked to adjudicate. In cases where studies reported outcome results over different time periods, we extracted data from each time period to examine the impact of the intervention over time. We followed the PRISMA guidelines in completing this systematic review [32]. 3. Results Figure 1 shows the flow of studies through the screening process. Nine hundred thirty-eight articles were captured during the initial literature search, of which 902 (96%) were excluded at the title and abstract screening stage. Full text screening was performed on 36 articles, of which only one was found to meet all the inclusion criteria. The reason for exclusion at the full-text screening stage was non-relevance of the article to our research objective (e.g., the outcomes of interest were not measured). Table 1 shows detailed study information for the only included study [33]. 3.1. Methodological Quality Assessment The included study, by Gitlin et al. [33], is an RCT in which outcome data were completely presented and no issues were evident with respect to selective reporting or any other type of bias. Overall, the study was rated as having a “low risk” of bias. Figure 1. Study flow diagram. A. A. Hazzan et al. 48 Table 1. Basic study description and data. Study Information Population Description Intervention Outcomes Gitlin (2003) Baseline = 255 Participants at 6 months: Int n = 89; Cntrl n = 101 Follow-ups: 6, 12 and 18 months post-baseline CR: behavioral problems; dependence in ADLs; dependence in IADLs USA CG: Caregiver well-being RCT Population Description at Baseline: Caregivers: Mean Age (SD): Int: 60.4 yrs (13.6) Cntrl: 60.5 yrs (13.6) % Male: Int 25%; Cntrl 23% Mastery: Caregiving Mastery Index Purpose: ESP–2 phases–active (first 6 months); maintenance (next 6 months) Care Recipient: Mean Age (SD): Int: 80.2 yrs (8.0) Cntrl: 81.5 yrs (8.0) % Male: Int 28%; Cntrl 37% Mean MMSE (SD): Int 11.6 (7.3); Cntrl 12.5 (7.1) Skill enhancement: Task Management Strategy Index CG = caregiver; CR = care recipient; ESP = environmental skill-building program; NH = nursing home; Int = intervention; Cntrl = control; MMSE = mini-mental state examination; ADL = Activities of daily living; IADL; Instrumental activities of daily living. 3.2. Summary of Extracted Study Although the included study was not specifically designed to answer our research questions, the data contained in the study did indirectly address whether caregiver QoL impacts the level or quality of care that caregivers provide to loved ones with AD. The Gitlin et al paper was primarily designed to examine the effect of an intervention (skills building program versus usual care) on caregiver well-being and care recipient functioning but contains sufficient information to examine the relationship between QoL and level/quality of care within groups of caregivers randomized into intervention and usual care control groups. Table 1 presents demographic information from the Gitlin et al. [33] paper that is relevant to the research questions in the current study. The population examined by Gitlin et al. consisted of 255 primary informal AD caregivers who were providing care for at least four hours per day for 6 months or more. The authors evaluated the impact of a Home Environmental Skill-Building Program (ESP) compared to a usual care control group. The ESP was designed to provide caregivers with education, problem-solving skills, and adaptive equipment to manage daily care challenges effectively and to reduce burdensome environmental stressors (e.g., CR behaviors) [33]. One hundred ninety caregivers completed six months of follow-up. As part of the study, the authors collected information about caregiver overall well-being, an important component of QoL [15] [33]. Caregiver overall well-being was measured with a 13-item scale (the Perceived Change Index [PCI]). On the PCI, caregivers used a 5-point scale to rate whether their situation (e.g., ability to manage difficult behaviors) ranged from “becoming worse” to “improving a lot” over the past month. The relevant level of care measure in the Gitlin et al. paper was caregiver time (the amount of time devoted to providing care and total hours of IADL help). The quality of care measures included caregiver mastery and skill enhancement. Caregiver mastery was measured with the Caregiving Mastery Index (CMI) [33]. The CMI is a six-item scale evaluating the caregiver’s appraisal of his or her ability to provide care to the CR (e.g., “How often do you feel you should be doing more for care recipient?). The scale uses a 5-point Likert format ranging from 1 (never) to 5 (always). A higher score means greater mastery of the care giving role. Skill enhancement was measured with the Task Management Strategy Index (TMSI), which is a 19-item scale that measures the extent to which positive care giving strategies were used to manage ADL dependence and problem behaviors in care recipients. The scale uses a 5-point Likert format from 1 (never) to 5 (always) [33]. 3.2.1. What Is the Relationship between Caregiver QoL and Level or Quality of Care Provided to Persons with AD? Table 2 shows the summary of data extracted from the included study. Overall, results from this study are A. A. Hazzan et al. 49 Table 2. Association between QoL and level/quality of care. Type of variable Measure Experimental Control BE 6ME Diff E BC 6MC Diff C QoL (Overall well-being) PCI 2.84 3.00 0.16 2.94 2.89 −0.05 Level of care Hours doing things for CR 12.23 11.51 −0.79 12.13 11.66 −0.47 Level of care Hours helping with IADLs 5.25 5.50 0.25 6.03 5.62 −0.41 Quality of care TMSI 2.91 3.05 0.14 2.92 2.93 0.01 Quality of care CMI 3.74 3.88 0.14 3.87 3.84 −0.03 E = Experimental; C = Control; CR = Care Recipient; QoL = Quality of Life; IADL = Instrumental Activities of Daily Living; PCI = Perceived Change Index; TMSI = Task Management Strategy Index; CMI = Care giving Mastery Index; B = Baseline; 6M = 6 month follow-up; Diff = Difference. mixed. We are primarily interested in whether changes in QoL are associated with changes in level or quality of care, within the experimental and the control group. Comparisons are described below: 3.2.2. Experimental vs Control Group: Baseline and 6-Month Follow-up Comparing the experimental group to the control group on outcomes related to level of care at baseline, results related to hours doing things for the CR are consistent with the hypothesis since lower QoL at baseline (before any intervention is given) is associated with higher number of hours spent caring for the CR (someone spending a lot of time providing care will have lower QoL). However, results for hours helping with IADLs do not support the hypothesis. Results for the quality of care variables (TMSI and CMI) are also consistent with the hypothesis. Compared to caregivers in the control group, lower QoL among caregivers in the intervention group is consistent with the lower quality of care that these caregivers provide at baseline. After 6 months of follow-up, there was an increase in the mean QoL among caregivers in the experimental group. On the other hand, there was a decrease in the mean QoL of caregivers in the control group over this period of time. Consistent with the hypothesis, there was an increase in the level (Hours helping with IADLs) and quality of care (TMSI and CMI) provided by caregivers in the intervention group compared to caregivers in the control group. The only exception to this trend is “hours doing things for CR”, which decreased among intervention group caregivers. 3.2.3. Experimental Group: Baseline to 6-Month Follow up Among caregivers in the experimental group, the QoL (PCI) variable increased over time. The overall results for this group from baseline to 6-months show that the experimental group QoL and quality of care measures increased over the follow-up period. On the other hand, results for the level of care variables are mixed, with hours doing things for CR showing a reduction over time, and hours helping with IADLs showing an increase over the same time period. The overall trend is consistent with the hypothesis since higher QoL at 6-month follow-up is related to higher level of care and quality of care. This means that caregivers with higher QoL are more likely to provide higher level of care and better quality of care. 3.2.4. Control: Baseline to 6-Month Follow up For caregivers in the control group, the QoL decreased over time from baseline to follow-up. The level of care and quality of care variables also decreased over time, with the only exception being TMSI which remains fairly constant over time. The observed trend is also consistent with the hypothesis since caregivers with lower QoL are likely to provide lower level and quality of care. Compared to caregivers in the control group, caregivers in the experimental group provided better care overall after 6-months follow-up. A. A. Hazzan et al. 50 3.3. Grade Results from the GRADE assessment are presented in Table 3. For both the level and quality of care outcomes, the type of evidence presented received the highest rating because the included study (Gitlin et al.) is an RCT and there were no serious issues with the quality of the study. However, the consistency, directness, and precision scores for both outcomes are affected by different factors, resulting in reduced scores on some of these domains. Consistency and directness points were deducted from both outcomes because the study was not designed to answer our research questions and results only indirectly addressed the questions. Finally, the precision scores were unchanged because the measures of effect were not statistically significant as reported in the included study [34]. 4. Discussion We were interested in evaluating how caregiver QoL impacts the level or quality of care that primary informal caregivers provide to their loved ones with AD. The included paper looks at level of care outcomes such as hours doing things for the CR and hours helping with IADLs. The paper also examine quality of care outcomes such as skill enhancement and caregiver mastery. Overall, the evidence was equivocal regarding the relationship between caregiver QoL and the level/quality of care provided to persons with AD. This is also the reason why the overall GRADE ratings for the outcomes from these studies are “moderate” This means that further research is likely to have an important impact on our confidence in this result [34]. Although the overall results were mixed, this study shows that higher caregiver QoL is related to higher level and quality of care provided to persons with AD. Among a group of 255 primary informal AD caregivers who were providing care for at least four hours per day for 6 months or more, findings at baseline show that caregivers spending a lot of time providing care were more likely to have lower QoL. This supports previous studies that have shown that caregiving in AD is stressful and has serious implications for the well-being of unpaid family caregivers [7]-[10]. In order to shed light on the relationship between QoL and level/quality of care provided to persons with AD, results for intervention and control group caregivers were analyzed after 6-months of follow-up. While there was an increase in the mean QoL among caregivers in the intervention group over the 6-month follow-up period, there was a decrease in the mean QoL of caregivers in the control group. As the QoL of intervention group caregivers increases over time, there was an increase in the level of care (Hours helping with IADLs) among these caregivers relative to caregivers in the control group. However, there was a decrease in the other level of care (Hours doing things for the CR) variable after 6-month of follow-up. It should be noted that “hours helping with IADLs” is a component of “total hours doing things for the CR” [33]. It is possible that “hours helping with IADLs” captures the important duties that AD caregivers perform for their loved ones better than “hours doing things for the CR”. At the same time, there was an increase in the quality of care (TMSI and CMI) provided by caregivers in the intervention group compared to those in the control group after 6-month follow-up. Although some specific results were mixed, the overall results supports the hypothesis that better caregiver QoL may lead to better level/quality of care for the CR. The mixed evidence from this systematic review suggests that research is needed to examine the relationship between caregiver QoL and the care provided to persons with AD. It is important to understand this relationship because our healthcare system places great responsibility on AD caregivers and we already know that AD caregivers’ QoL is lower than other caregivers’ QoL. Considering the critical duties that caregivers of persons with Table 3. Grade results. Outcome Type of evidence Quality Consistency Directness Precision GRADE Notes Level of care (hours helping care recipient, hours helping with IADLs) 4 0 −1 −1 0 Moderate Directness point deducted because results indirectly address review questions Quality of care (TMSI, CMI) 4 0 −1 −1 0 Moderate Consistency point deducted because only one trial examined the intervention IADL = Instrumental Activities of Daily Living; TMSI = Task Management Strategy Index; CMI = Care giving Mastery Index. A. A. Hazzan et al. 51 AD perform, the current systematic review shows an urgent need for studies examining the relationships between caregiver QoL and the level/quality of care. The ideal type of primary study to address our research questions is a longitudinal cohort study measuring QoL, level of care, and quality of care in AD caregivers. If such a study were to be conducted, the longitudinal component will show how the relationship between variables changes as caregiver QoL deteriorates over time. The Canadian Longitudinal Study on Aging (CLSA) is a model for the types of studies that could be used to collect the data needed to answer our research questions [35] [36]. If the results from a longitudinal study show that caregivers’ QoL does indeed affect their ability to provide care for their loved ones with AD, then this issue needs to be addressed through additional support programs that improve caregiver QoL. For example, respite care and similar alternative care options could be made more available to relieve caregivers of persons with AD from their care giving duties. Further, programs could be designed to help caregivers address day-to-day challenges such as financial and legal planning, stress management, and behavioural interventions. Access to educational interventions that help caregivers acquire valuable skills would also improve the care giving experience. 5. Limitations One limitation of this systematic review is that the only study that met the inclusion criteria provided indirect evidence to answer the research questions. Also, because primary data were not available, it was not possible to determine if the observed relationships between caregiver QoL and level/quality of care are statistically significant or not. However, this systematic review makes an important contribution to the literature because it shows that very little research has been conducted into the relation between QoL and level/quality of care. The review highlights the need for additional research in this area. 6. Conclusion As population aging continues to occupy a more prominent role in research and policy discussions, more attention needs to be given to the situation of unpaid family caregivers of persons with AD. Family caregivers play an important role in the management of AD and several studies have shown that these caregivers experience lower QoL compared to the QoL experienced by caregivers of persons who do not have AD. This systematic review shows that there is insufficient evidence regarding the nature of the relationship between unpaid family caregiver QoL and level/quality of care provided to persons with AD. Considering the important duties that caregivers of persons with AD perform, additional research should be conducted to examine this relationship. Acknowledgements The authors would like to thank Mary Gauld for helping with Distiller and article screening. We thank Maureen Rice for helping with developing the literature search strategies and conducting the literature search. We also thank Vincent Wu and Arnav Agarwal for helping with article screening. References [1] Alzheimer’s Disease International (2011) World Alzheimer Report 2011. The Benefits of Early Diagnosis and Intervention. Alzheimer’s Disease International, London. http://www.alz.co.uk/research/world-report-2011/ [2] Burns, A. and Iliffe, S. (2009) Alzheimer’s Disease. British Medical Journal, 338, 46-471. http://dx.doi.org/10.1136/bmj.b46 [3] Hebert, L.E., Scherr, P.A., Bienias, J.L., Bennett, D.A. and Evans, D.A. (2003) Alzheimer disease in the US Population: Prevalence estimates Using the 2000 Census. Archives of Neurology, 60, 1119-1122. http://dx.doi.org/10.1001/archneur.60.8.1119 [4] Alzheimer Society of Canada (2012) Key Facts about Alzheimer’s Disease and Related Dementia-Prevalence Figures. Alzheimer Society of Canada, Toronto. http://www.alzheimer.ca/english/disease/stats-intro.htm [5] Canadian Study of Health and Aging (1994) Canadian Study of Health and Aging: Study Methods and Prevalence of Dementia. Canadian Medical Association Journal, 150, 899-913. [6] Prince, M. and Jackson, J. (2009) Alzheimer’s Disease International: World Alzheimer Report. A. A. Hazzan et al. 52 http://www.alz.co.uk/research/world-report [7] deMoraes, S.R. and da Silva., L.S. (2009) An Evaluation of the Burden of Alzheimer Patients on Family Caregivers. Cadernos de Saúde Pública, 25, 1807-1815. [8] Schulz, R., Belle, S.H., Czaja S.J, McGinnis, K.A., Stevens, A. and Zhang, S. (2004) Long-Term Care Placement of Dementia Patients and Caregiver Health and Well-Being. The Journal of the American Medical Association, 292, 961-967. http://dx.doi.org/10.1001/jama.292.8.961 [9] Port, C.L., Zimmerman, S., Williams, C.S., Dobbs, D., Preisser, J.S. and Williams, S.W. (2005) Families Filling The Gap: Comparing Family Involvement for Assisted Living and Nursing Home Residents with Dementia. Gerontologist, 1, 87-95. [10] Zarit, S.H., Orr, N.K. and Zarit, J.M. (1985) The Hidden Victims of Alzheimer’s Disease: Families under Stress. New York University Press, New York. [11] Bolge, S.C., Doan, J.F., Kannan, H. and Baran, R.W. (2009) Association of Insomnia with Quality of Life, Work Productivity, and Activity Impairment. Quality of Life Research, 18, 415-422. http://dx.doi.org/10.1007/s11136-009-9462-6 [12] Gaugler, J.E., Yu, F., Krichbaum, K. and Wyman, J.F. (2009) Predictors of Nursing Home Admission for Persons with Dementia. Medical Care, 47, 191-198. http://dx.doi.org/10.1097/MLR.0b013e31818457ce [13] Alzheimer’s Association and National Alliance for Care Giving (2004) Families Care: Alzheimer’s Disease Care Giving in the United States. www.alz.org [14] Hazzan, A.A., Ploeg, J., Shannon, H., Raina, P., Oremus, M. (2013) Association between Caregiver Quality of Life and the Care Provided to Persons with Alzheimer’s Disease: Protocol for a Systematic. Systematic Review, 13, 17. [15] World Health Organization (WHO) (1997) Measuring Quality of Life. WHOQOL. World Health Organization, Geneva. [16] Susniene, D. and Jurkauksa, A. (2009) The Concepts of Quality of Life and Happiness—Correlation and Differences. Engineering Economics. [17] McSweeny, A.J. and Creer, T.L. (1995) Health-Related Quality-Of-Life Assessment in Medical Care. Diseasea-Month, 41, 1-71. [18] Ware, J.E. and Sherbourne, C.D. (1992) The MOS 36-Item Short-Form Health Survey (SF-36) Conceptual Framework and Item Selection. Medical Care, 30, 473-483. http://dx.doi.org/10.1097/00005650-199206000-00002 [19] EuroQol Group (1990) EuroQol—A New Facility for the Measurement of Health-Related Quality Of Life. The Euro Qol Group. Health Policy, 16, 199-208. http://dx.doi.org/10.1016/0168-8510(90)90421-9 [20] Saxena, S. and Orley, J. (1997) Quality of Life Assessment: The World Health Organization Perspective. European Psychiatry, 12, 263s-266s. http://dx.doi.org/10.1016/S0924-9338(97)89095-5 [21] Markowitz, J.S., Gutterman, E.M., Sadik, K. and Papadopoulos, G. (2003) Health-Related Quality of Life for Caregivers of Patients with Alzheimer Disease. Alzheimer Disease and Associated Disorders, 17, 209-214. http://dx.doi.org/10.1097/00002093-200310000-00003 [22] Bédard, M., Molloy, D.W., Squire, L., Dubois, S., Lever, J.A. and O’Donnell, M. (2001) The Zarit Burden Interview: A New Short Version and Screening Version. Gerontologist, 41, 652-657. http://dx.doi.org/10.1093/geront/41.5.652 [23] Ferro, M.A. and Speechley, K.N. (2009) Depressive Symptoms among Mothers of Children with Epilepsy: A Review of Prevalence, Associated Factors, and Impact on Children. Epilepsia, 50, 2344-2354. http://dx.doi.org/10.1111/j.1528-1167.2009.02276.x [24] Radloff, L.S. (1977) The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement, 1, 385-401. http://dx.doi.org/10.1177/014662167700100306 [25] Niedhammer, I., David, S. and Degioanni, S. (2006) Association between Workplace Bullying and Depressive Symptoms in the French Working Population. Journal of Psychosomatic Research, 61, 251-259. http://dx.doi.org/10.1016/j.jpsychores.2006.03.051 [26] Teri, L., McCurry, S.M., Logsdon, R. and Gibbons, L.E. (2005) Training Community Consultants to Help Family Members Improve Dementia Care: A Randomized Controlled Trial. Gerontologist, 45, 802-811. http://dx.doi.org/10.1093/geront/45.6.802 [27] McCurry, S.M. and Teri, L. (1995) Sleep Disturbance in Elderly Caregivers of Dementia Patients. Clinical Gerontologist, 16, 51-66. http://dx.doi.org/10.1300/J018v16n02_05 [28] Higgins, J.P., Altman, D.G., Gøtzsche, P.C., Jüni, P., Moher, D., Oxman, A.D., Savovic, J., Schulz, K.F., Weeks, L., Sterne, J.A., Cochrane Bias Methods Group and Cochrane Statistical Methods Group. (2011) The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. British Medical Journal, 343, d5928. http://dx.doi.org/10.1136/bmj.d5928 A. A. Hazzan et al. 53 [29] Cochrane Effective Practice and Organisation of Care Group Draft Risk of Bias Tool (2011) Wiley, Oxford. http://epoccochrane.org/epocresources-review-authors [30] Hartling, L., Bond, K., Harvey, K., Santaguida, P.L., Viswanathan, M. and Dryden, D.M. (2010) Developing and Testing a Tool for the Classification of Study Designs in Systematic Reviews of Interventions and Exposures. http://www.ncbi.nlm.nih.gov/books/NBK52670/pdf/TOC.pdf [31] The Cochrane Handbook for Systematic Reviews of Intervention. (2011) The GRADE Approach. Chapter 12.2.1. http://handbook.cochrane.org/chapter_12/12_2_1_the_grade_approach.htm [32] Moher, D., Liberati, A., Tetzlaff, J. and Altman, D.G. (2010) PRISMA Group: Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. International Journal of Surgery, 8, 336-341. http://dx.doi.org/10.1016/j.ijsu.2010.02.007 [33] Gitlin, L.N., Winter, L., Corcoran, M., Dennis, M.P., Schinfeld, S. and Hauck, W.W. (2003) Effects of the Home Environmental Skill-Building Program on the Caregiver-Care Recipient Dyad: 6-Month Outcomes from the Philadelphia REACH Initiative. Gerontologist, 43, 532-546. http://dx.doi.org/10.1093/geront/43.4.532 [34] Guyatt, G.H., Oxman, A.D., Vist, G.E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., Schünemann, H.J. and GRADE Working Group. (2008) GRADE: An Emerging Consensus on Rating Quality of Evidence and Strength of Recommendations. British Medical Journal, 336, 924-926. http://dx.doi.org/10.1136/bmj.39489.470347.AD [35] Canadian Study of Health and Aging Working Group. (2000) The Incidence of Dementia in Canada. Neurology, 55, 66-73. http://dx.doi.org/10.1212/WNL.55.1.66 [36] Raina, P.S., Wolfson, C., Kirkland, S.A., Griffith, L.E., Oremus, M., Patterson, C., Tuokko, H., Penning, M., Balion, C.M., Hogan, D., Wister, A., Payette, H., Shannon, H. and Brazil, K. (2009) The Canadian Longitudinal Study on Aging (CLSA). Canadian Journal on Aging, 28, 221-229. http://dx.doi.org/10.1017/S0714980809990055


